▼What is breast cancer?
Cells in your breast can change and no longer grow or behave ‘normally’. These changes may lead to non-cancerous (benign) breast conditions (such as cysts, atypical hyperplasia, intraductual papillomas etc.). But in some cases, changes to your breast cells can lead to breast cancer1.▼Canadian statistics
Breast cancer is the second most common form of cancer diagnosed in women, after skin cancer. It accounts for 25% of all new cancer cases in women2. The 5-year survival rate for breast cancer in women is 89% (i.e., on average, 89% of women diagnosed with breast cancer will live for at least 5 years3). Survival varies with each stage* of breast cancer, and for different patient demographics. Generally, the earlier breast cancer is diagnosed and treated, the better the outcome.3*Staging is a way of describing how extensive the breast cancer is, including the size of the tumor, whether it has spread to lymph nodes, whether it has spread to distant parts of the body, and what its biomarkers are4.
▼Risk factors
Your risk of developing breast cancer generally increases with age, peaking around 69 years of age5. Additional risk factors include5,6:- Personal history of breast cancer
- Family history of breast cancer and other cancers
- BRACA gene mutations
- Dense breasts7
- Alcohol consumption
- Late or no pregnancies
- Radiation exposure
- Hormone replacement therapy
- Poor general health (e.g., obesity, physical inactivity, smoking etc.)
- Post-menopausal
- If you have never breast fed
- Being a minority population (including Indigenous8 , South Asians9 , Blacks10 , and recent immigrants11), who are often diagnosed at later stages of breast cancer and therefore have a lower chance of survival (higher mortality rate)
▼Screening
Provincial and territorial screening programs use mammography, a low-dose x-ray of the breast. Screening mammography is good at finding breast cancer. Overall, the sensitivity of mammography is 87%. This means that mammography correctly identifies about 87% of women who have breast cancer12. Regular mammograms can help to identify abnormal breast cells at early stages, which will increase your survival rate13. You should be aware of the benefits and limitations of screening mammography based on your age and risk factors to help decide if and when it is right for you.Current Canadian screening recommendation are13:
- If you are 40 to 49 years old, talk to your doctor about your risk for breast cancer, along with the benefits and limitations of having a mammogram
- If you are 50 to 74 years old, have a mammogram every 2 years
- If you are 75 or older, talk to your doctor about if having a mammogram is right from you
However, screening guidelines do vary depending on the province or territory. For example, Ontario lowered their screening age to 40, consistent with BC and NS, as well as the US, who recently changed their national recommendation to begin breast screening at age 40, with mammography every two years. Previously, like current Canadian national recommendations, women were advised to start at age 50 and those in their 40s were told to make an individual decision. The US Preventative Service Task Force made the recommendations for earlier screening in hope of saving lives, especially of black women who are 40% more likely to die of breast cancer than white women and too often get deadly cancers at younger ages.14,15 In agreement to this recent US change, a 2023 Canadian publication by Dr. Yong-Hing discussed how Canada’s minimum screening age should also be reduced to 40s, with yearly screening of asymptomatic women aged 40-49. This is based on the most recent clinical evidence, which was not included during the last Canadian guideline update in 2018.16
The Canadian Task Force on Preventative Health Care is currently undergoing an expedited review process to inform how they will update their guidelines.17
▼Diagnosis
Diagnosis is the next step following an abnormal finding in your screening mammography or when you find a lump in your breast (it is important to see your doctor if you detect an abnormality). This may involve examining the affected area using a non-invasive diagnostic imaging technique such as ultrasound, magnetic resonance imaging (MRI), or mammogram (x-ray). These tests can be sufficient in aiding a doctor with their diagnosis, however if still unsure, they may opt to perform a breast biopsy18. In contemporary practice, most palpable lumps deemed suspicious on diagnostic imaging are biopsied with imaging guidance.18 A biopsy is the only procedure that can determine whether a breast lump is cancerous19. The type of biopsy performed will be determined by your health care professional. As a potential biopsy patient, do not hesitate to ask your health care provider as many questions as you need, to understand the procedures that you have been booked for. Although finding a lump in your breast or the thought of a biopsy may be worrying at first, it is worth knowing that 80% of women who undergo a biopsy do not have breast cancer20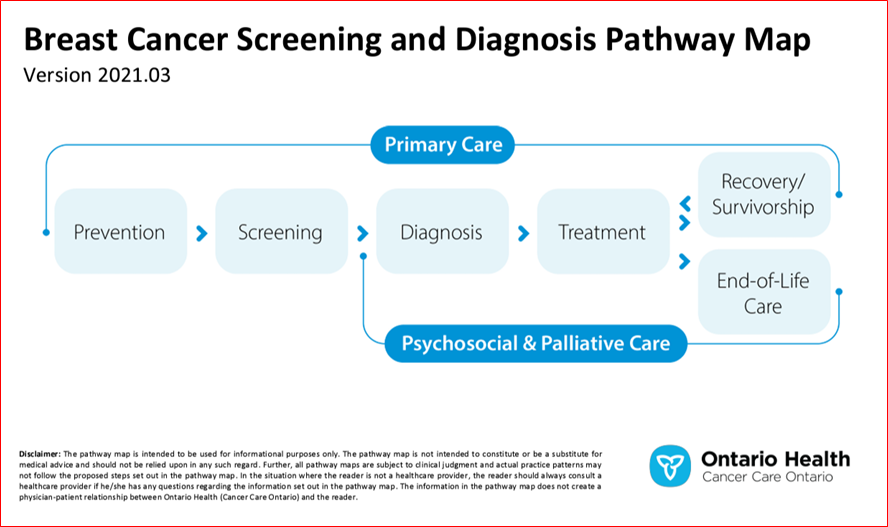 |
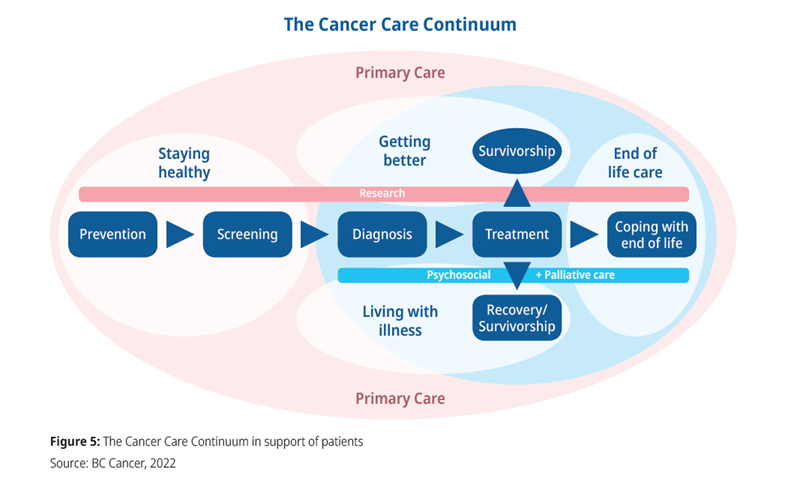 |
| Example of a provincial screening and diagnosis pathway. Each patient’s actual path may differ depending on their individual’s circumstances.21 |
|
For additional resources please visit: